Absolute transparency vital in every health emergency
The Social Health and Family Affairs Committee of the Parliamentary Assembly, Council of Europe published an important report titled ‘The Handling of the H1N1 Pandemic—More Transparency Needed’.
Galen’s principal interest was in human anatomy, but Roman law had prohibited the dissection of human cadavers. So he performed them on living and dead animals as he believed that these were the same as humans. His anatomical experiments on animal models led him to propound on the circulatory, nervous, respiratory systems and other structures — all of which turned out to be entirely incorrect.
Claudius Galenus, known as Galen was a Greek physician/ surgeon in the Roman empire, and was physician to several Roman emperors. He, unfortunately, influenced the development of various scientific disciplines, including anatomy, physiology, pathology, pharmacology and neurology, in European medical science for 1300 years, till proper scientists found that everything he said was “incorrect” or rubbish.
Galen’s anatomical reports, based mainly on dissection of monkeys and pigs, remained uncontested until 1543, when printed descriptions and illustrations of human dissections were published in the seminal work De Humani Corporis Fabrica by Andreas Vesalius, who had conducted dissection on human cadavers which turned out to be completely different. Galen’s theory of the circulatory system remained unchallenged until ca. 1242, when Ibn al-Nafis published his book Sharh Tashrih al-Qanun li’ Ibn Sina (Commentary on Anatomy in Avicenna’s Canon), in which he reported his discovery of pulmonary circulation, proving Galen completely wrong.
Advertisement
Galen’s principal interest was in human anatomy, but Roman law had prohibited the dissection of human cadavers. Because of this restriction, Galen performed anatomical dissections on living and dead animals, as he believed that these were the same as humans. His anatomical experiments on animal models led him to propound on the circulatory, nervous, respiratory systems and other structures – all of which turned out to be entirely incorrect. Galen killed thousands of people using the theories deduced from killing thousands of animals.
Advertisement
Unfortunately, while all these theories, gleaned from killing animals, were proved wrong, his legacy of testing on animals remains prevalent till today, even though it has been proven again and again that animal-based experiments have not contributed to science, but rather have hindered scientific and medical progress. As a matter of fact, most of the major life saving devices and procedures came without anything to do with animals. Take the heart, for example:
Dogs’ coronary arteries differ from humans. They have smaller connections with one another and the left coronary artery dominates, while in the human the right artery dominates. The conduction system has a different pattern of blood supply. Dogs’ blood coagulates differently from humans. Their reaction to shock is different. After massive blood loss, a dog’s intestines are congested, while in the human we see pallor and ischemia (lack of blood supply). But we continue to experiment on dogs.
Here is a list of major discoveries made without animal experimentation:
Anesthesia: Ether was discovered by Valerius Cordus in 1540, when he mixed alcohol and sulphuric acid. Called “sweet oil of vitriol”, Medical students used ether to get high in “ether frolics”. Dr. Crawford Long, a surgeon, noticed that people with bruises who had taken ether were insensitive to pain. He tried it on a patient during surgery.
Hypothermia – (cooling the body before surgery): In 1757 observation of persons exposed to cold for long periods showed that they could survive, and was written about by the Swedish Academy of Sciences. In 1798 Dr. James Currie had human volunteers take prolonged baths in cold water. He discovered that their heart rate was reduced. This information is now used to reduce the heart rate in patients before surgery.
Positive pressure ventilation- (blowing air into the lungs during surgery): Dr. Ferdinand Sauerbrach created positive pressure ventilation to keep the lungs from collapsing during surgery, but withdrew the technique when it proved harmful to animals. In 1891 American surgeon George Fell decided to use it anyway, and used it successfully.
Heart lung machine- Dr. Jack Gibbon tested it on cats, then humans. The humans died. Then other doctors perfected it while using it on human patients. Dr. Anthony Andreason created the low flow theory – that less blood would have to be used than the amount in the body, by observing that war injured soldiers could survive on less blood than originally thought.
Heart pacemakers- Grew out of ventricular septal defect surgery. To prevent deaths during heart surgery, due to stoppage of electrical activity, the pacemaker was developed to keep the electrical activity going and to keep the heart from giving out.
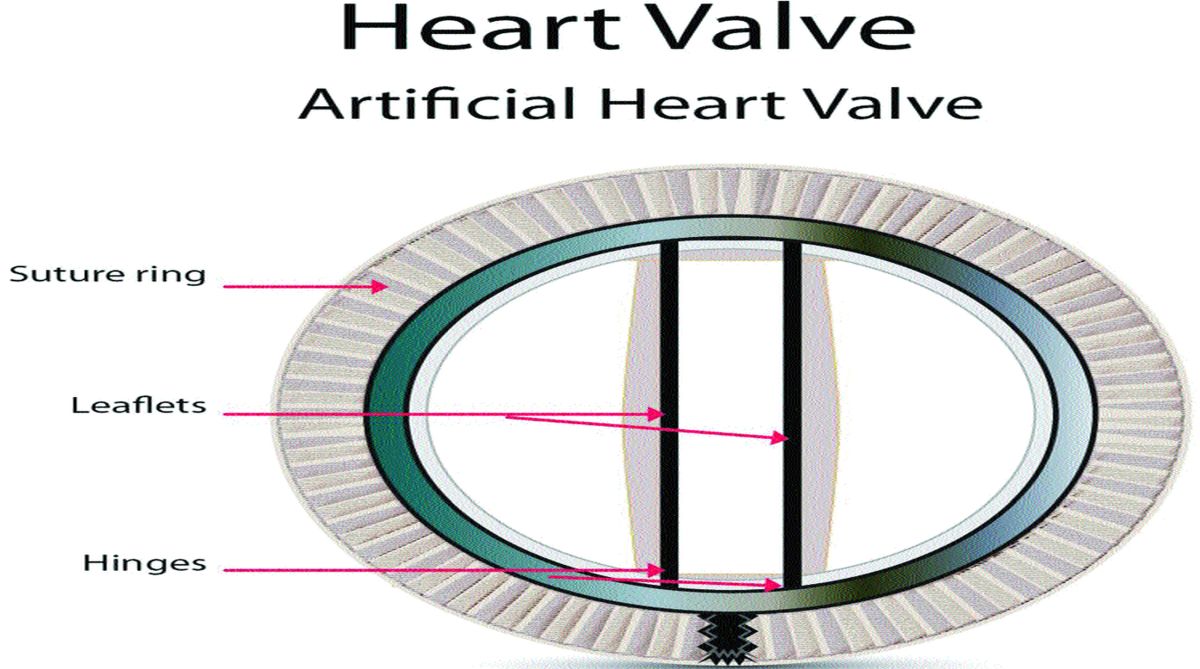
Artificial heart valves- The cage ball valve was almost withheld from human patients because it killed dogs in the lab. Drs. A. Starr and L. Edwards found that it worked on humans.
Blood transfusions- In 1667, Jean Dennis transfused blood from animals to humans and killed people. Blood typing was discovered by an American scientist without animal experiments, and that led to successful blood transfusions.
Cardiac catherization- (for diagnostic purposes): First used by Dr. Forsmann on himself. He put a catheter through his own arm and advanced the tip to his heart, observing it through a fluoroscope.
Bypass surgery- In 1961, in France, Dr. Kunlin used a portion of a person’s vein to replace obstructed segments. This gave birth to bypass surgery for different parts of the body.
Calcium antagonists- (used to treat high blood pressure): It was discovered to lower the blood pressure when given to patients to reduce heart pain (angina).
Bubble oxygenator- C Walton Lillehei developed it through learning what happened to patients during surgery when the heart lung machine was used and complications arose. He decided to use the disposable sheet oxygenator, so that blood would not become contaminated.
Anti-foaming agents- (used to stop blood from bubbling when oxygen is put into it): Was developed to stop milk from foaming, and adapted to use in open heart surgery.
Coarctation of the aorta- (twisting of the aorta that prevented blood flow): Clarence Crafford put a clamp on the ruptured aorta and discovered that he could still perform surgery on the aorta without the patient dying. He discovered this by accident on a patient.
Mitral stenosis- (defective heart valve): Dr. Henry S. Souttar, London Hospital, 1925, put his forefinger through the heart’s mitral valve and widened it. In 1949 Dr. Dwight E. Harking decided to use that same technique which is called finger fracture angioplasty.
Blue babies- (Fallot’s Tetrology – Four heart defects that lead to blue baby syndrome): Dr. R C Brock of Guy’s Hospital developed a technique of surgery to overcome this problem, without any animal experiments (British Medical Journal 6/12/48). Another technique was developed by British surgeons N. R. Barrett and Raymond Daley of St. Thomas Hospital (British Medical Journal 4/23/49).
Cardiopulmonary resuscitation- Kouwenhoven, Jude and Knickerbocker devised this technique through practice on cadavers.
Closed chest cardiac resuscitation- Dr. Paul Zoll used this technique (electric shock) as early as 1956.
Electrocardiogram- Brown and Mac Millan, Toronto, began investigating arrhythmia disorders directly on patients. Converted an old encephalogram to an electrocardiogram to monitor heart rhythm disorders.
Digitalis- Dr. Thomas Lewis, Great Britain: “The most essential information, the profound effects which digitalis is capable of exerting in auricular fibrillation, could not have been won through observation on the frog or normal mammal, but only, as it was won, by observation on patients.”
To join the animal welfare movement contact gandhim@nic.in, www.peopleforanimalsindia.org
Advertisement