One answer to food crisis may lie beneath our feet
After a sizzling summer, the UN Secretary General has warning that the “era of global boiling has arrived” Climate change…
When the patient required anesthesia following successful resuscitation, midazolam increased the likelihood of adequate oxygen saturation and CO2 levels in the blood.
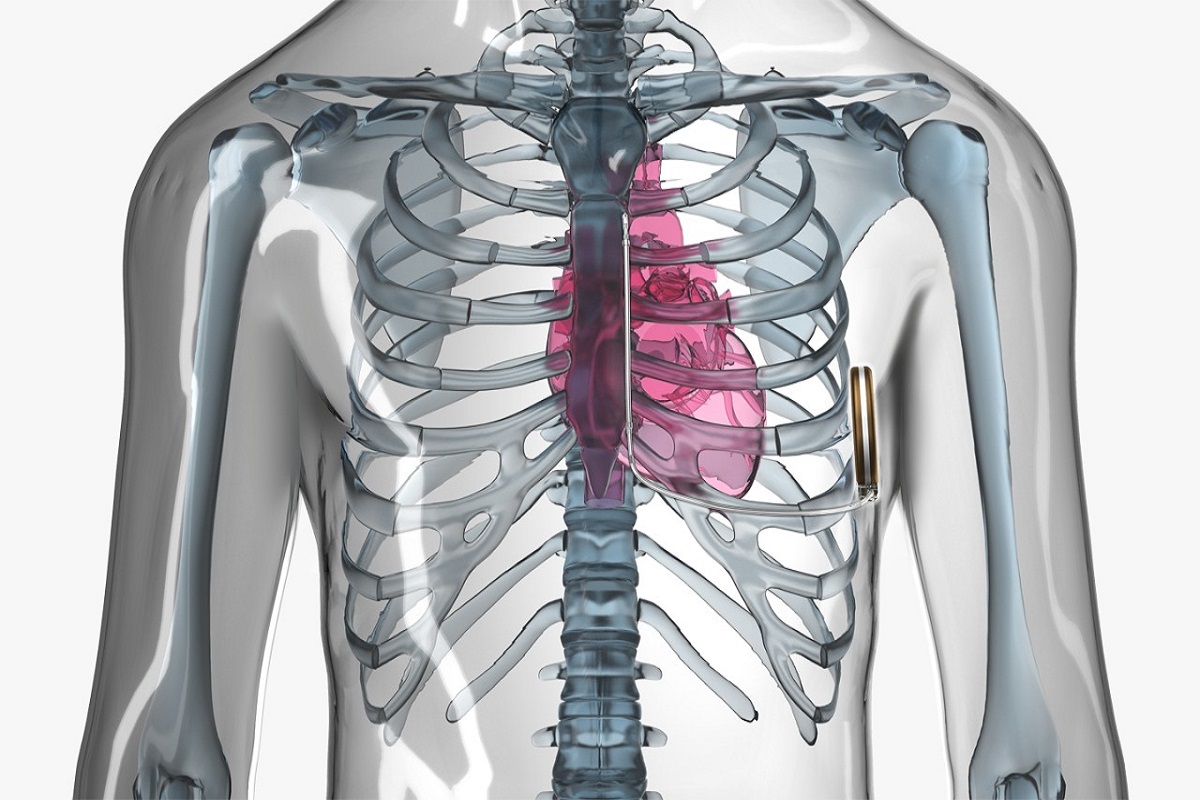
cardiac arrest
When the patient required anesthesia following successful resuscitation, midazolam increased the likelihood of adequate oxygen saturation and CO2 levels in the blood. The risk of a subsequent decline in blood pressure or circulatory arrest did not increase.
“This particular group of patients who have been successfully resuscitated should undoubtedly be included in the pre-hospital anaesthesia guidelines. Dr Gerrit Jansen, lead author of the study published in Deutsches Arzteblatt International, believes that midazolam has a particularly good effect in this group of patients.
In the event of a cardiac arrest, rapid intervention is essential: If first aiders carry out resuscitation measures in good time, the patient’s circulation can be restarted in the best-case scenario. “However, it’s often the case that the patient hasn’t yet regained consciousness,” explains Gerrit Jansen. In this phase, there are various factors that can affect the chances of survival and subsequent permanent limitations due to the circulatory arrest.
Advertisement
“Some patients display protective reflexes after resuscitation, such as coughing or defensive movements, which make the emergency responders’ work more difficult. They often have to perform extended airway management, for example by intubating the patient in the same way as during surgery. This frequently requires sedation or anesthesia,” explains Jansen. Until now, there has been concern that anaesthetic drugs could have a negative impact on the circulatory system, which has only just been restored. According to the study, however, this is not the case.
Advertisement
Of the 571 people included in the study who survived a cardiac arrest and were admitted to hospital, 395 were sedated, 249 of them with midazolam. The chance that their blood oxygen saturation levels were in the optimal range following a cardiac arrest increased twofold when midazolam was administered. The chance that carbon dioxide was effectively exhaled increased by a factor of 1.6 with the drug. “Our statistical methods confirmed a correlation between these results and the administration of midazolam, without any indication of negative circulatory effects,” says Gerrit Jansen.
“The European guidelines of the European Resuscitation Council don’t yet set out any specific recommendations for possible anesthetic drugs,” explains Jansen. “The German guideline for pre-hospital anesthesia for patients with cardiovascular risk doesn’t mention patients in cardiac arrest. We’ve therefore carried out pioneering research in this field, the results of which should be incorporated into the recommendations for the benefit of the patients.”
Advertisement